Introduction
Chimeric antigen receptor (CAR) T-cells can induce a rapid disease response but are frequently associated with immunologic toxicities. In addition to cytokine release syndrome (CRS), macrophage activation syndrome-like manifestations (MAS-L), characterized by uncontrolled immune activation, have been described (Shah et al, 2020). Traditional MAS definitions are challenging to apply in patients receiving CAR T cells, due to overlapping signs and symptoms with lymphodepletion and CRS. Therefore, we sought to develop novel criteria to characterize MAS-L following CAR T cells and used these criteria to identify risk factors for developing MAS-L.
Methods
We conducted a retrospective review of 55 patients who received B cell maturation antigen-directed CAR T cells for multiple myeloma from 11/1/17 - 5/1/20. Based on the labs readily available in our patient population, we defined MAS-L using the following criteria: 1) rate of ferritin rise ³ 100 mg/L/hour within a 24 hour period and2) minimum fibrinogen < 150 mg/dL or maximum LDH > 2 times the upper limit of normal. In developing these simplified criteria, we considered multiple laboratory markers of inflammation (ferritin, LDH, soluble interleukin receptor-2, natural killer cell activity) and end organ damage. Infection was defined as any culture positivity, febrile neutropenia, or clinical suspicion such that a new antimicrobial was started in the 30 days prior to CAR T cells. Wilcoxon rank-sums and Fisher's exact test were used to compare continuous and categorical variables, respectively. Overall (OS) and progression-free survival (PFS) were compared using log-rank tests.
Results
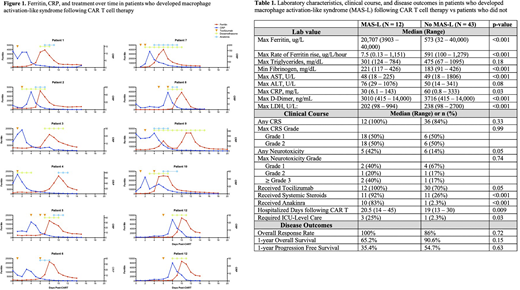
Of the 55 patients, 12 (21.8%) met the above criteria for MAS-L with similar disease trajectories. Following CAR T cells, all 12 patients first developed CRS, characterized by an elevated C-reactive protein (CRP) and administration of tocilizumab, and subsequently developed MAS-L, characterized by decrease in fibrinogen and rapid rise of ferritin and LDH (Figure 1).
Compared to the 45 patients who did not develop MAS-L, patients with MAS-L had similar baseline patient and disease characteristics (Table 1); however, a significantly higher proportion of patients with MAS-L had an infection prior to receiving CAR T cells (75% vs 9.3%, p < 0.001.) Patients with MAS-L also had higher peak ferritin (median 20,707 vs 573 ug/L, p < 0.001), D-dimer (14,000 vs 3,010 ng/mL, p < 0.001), aspartate aminotransferase (AST; 153 vs 48 U/L:, p < 0.001) and a trend towards higher alanine aminotransferase (ALT; 76 vs 50 U/L, p = 0.08). In contrast, patients with MAS-L had a lower peak C-reactive protein (CRP; 29.8 vs 60 mg/L, p = 0.03).
Compared to patients who did not develop MAS-L, a similar proportion of MAS-L patients developed any CRS (100% vs 84%, p = 0.33) and ³ grade 2 CRS (50% vs 50%, p = 1). Neurotoxicity was more common in patients with MAS-L (42% vs 14%, p = 0.05). A greater proportion of patients with MAS-L received tocilizumab (100% vs 70%, p = 0.05), systemic steroids (92% vs 27%, p < 0.001), and anakinra (83% vs 2.3%, p < 0.001). Anakinra was given per clinician discretion and not per study protocol.
Following CAR T cell therapy, patients with MAS-L had longer hospitalizations (21 vs 19 days, p = 0.009) and a greater proportion required ICU-level care (27% vs 2%, p = 0.02). OS and PFS between the two groups were similar (p = 0.15 and 0.63, respectively), with a 1-year OS of 65.2% vs 90.6% and PFS of 35.4% vs 54.7% for patients with vs without MAS-L, respectively.
In univariate logistic regression of baseline patient factors, disease characteristics, and ferritin, CRP, and D-dimer prior to receiving CAR T cells, only a history of documented infection in the 30 days prior to CAR T cells predicted MAS-L development (Hazard Ratio 29.2, 95% CI 5.54 - 154, p < 0.001).
Conclusions
In this analysis, we developed novel criteria for defining MAS-L following CAR T cell therapy and used these criteria to define the unique laboratory profile and clinical trajectory of patients with MAS-L. We also identify pre-existing infection as a strong risk factor for MAS-L development. Although patients with MAS-L frequently require prolonged monitoring, this immunologic toxicity can be mitigated with steroids, anakinra, and supportive care, and patients ultimately have similar survival compared to patients without MAS-L. Larger studies are needed to prospectively validate these novel criteria.
Wolf:Adaptive: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Martin:Sanofi, Amgen, Seattle Genetics, JNJ - Janssen: Research Funding; Legend Biotech: Consultancy. Shah:BMS, Janssen, Bluebird Bio, Sutro Biopharma, Teneobio, Poseida, Nektar: Research Funding; GSK, Amgen, Indapta Therapeutics, Sanofi, BMS, CareDx, Kite, Karyopharm: Consultancy. Wong:Bristol Myers Squibb: Research Funding; Sanofi: Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy; Janssen: Research Funding; Roche: Research Funding; Fortis: Research Funding; GSK: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal